What is Diabetic Foot
Diabetic foot conditions are a critical concern that demand vigilant care and awareness, not only from those diagnosed with diabetes but also from their caregivers and healthcare providers. The implications of diabetic foot range from mild infections to severe complications that can lead to amputation or worse. It is crucial to recognize that diabetic foot is not merely a symptom of diabetes but a stark indicator of the broader health challenges that diabetes can provoke.
For a diabetic, the foot becomes a litmus test for how well the condition is being managed. High blood sugar levels associated with uncontrolled diabetes can cause damage to the blood vessels and nerves, leading to neuropathy (nerve damage) which diminishes sensation in the feet. This loss of sensation is perilous because it can prevent the detection of injuries, leading to complications that might not be noticed until they become extremely severe.
However, what is often less discussed is the psychological and emotional toll that diabetic foot can take on individuals. The constant vigilance over foot health can induce significant stress, anxiety, and in some cases, depression. The fear of amputation or severe infection can alter a person’s lifestyle, making them more hesitant to engage in activities they once enjoyed. Furthermore, the changes in foot appearance and function can affect self-esteem and social interactions, deepening the psychosocial impact of the condition.
Understanding Diabetic Foot
The complexity of diabetic foot conditions requires not just a knowledge of symptoms but also a deep understanding of the mechanisms that lead to these critical issues. This understanding is crucial for implementing effective preventative and treatment strategies. A pivotal resource in this realm is the article titled “Comprehensive Foot Examination and Risk Assessment,” published by the American Diabetes Association in the journal Diabetes Care. This article meticulously outlines the essential steps in examining and assessing the risk of foot complications in diabetic patients. Read more about the recommendations.
Definition and Causes
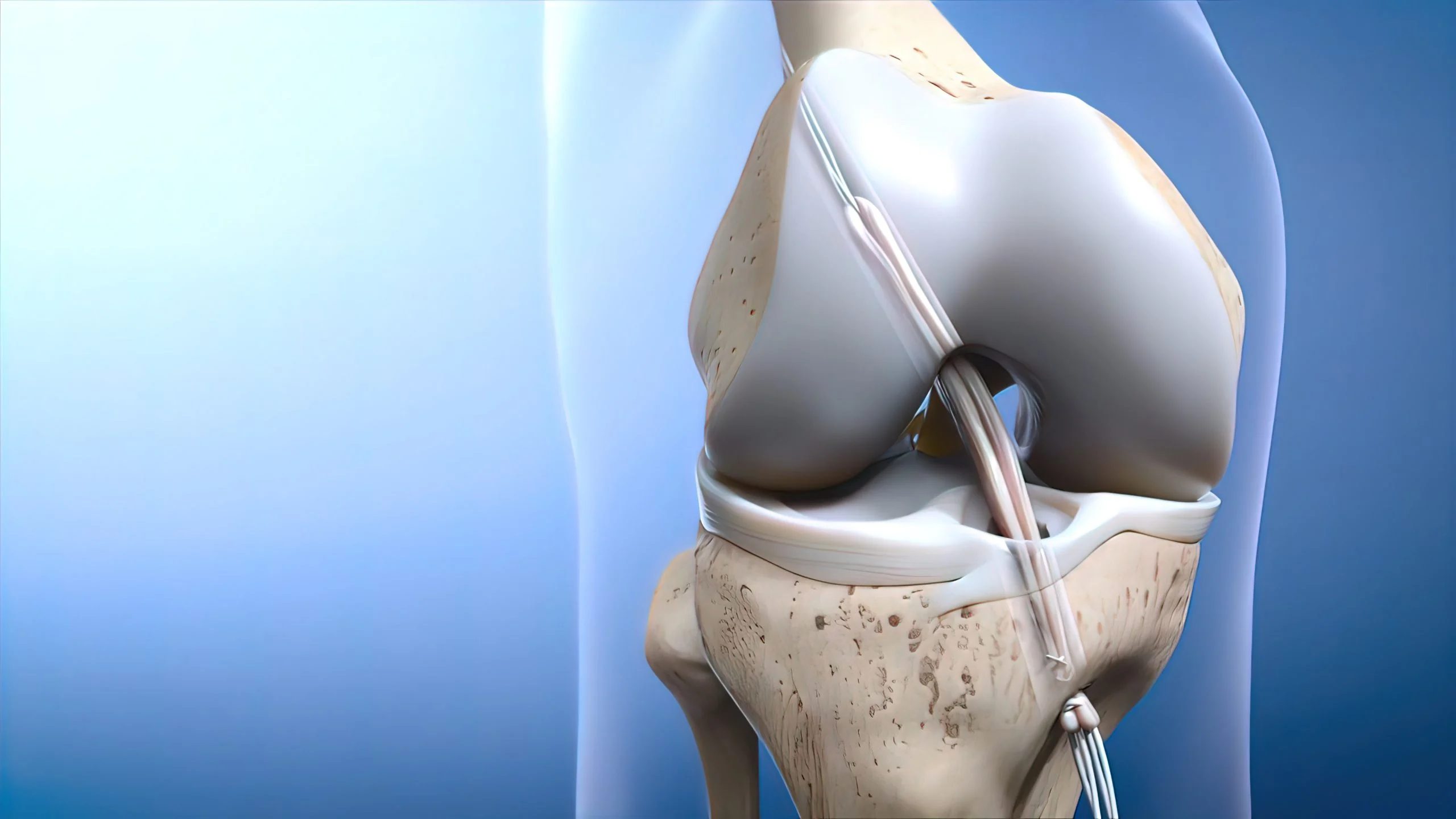
Diabetic foot refers to serious complications arising from diabetes, including infections, ulcerations, and potential limb amputation. These complications are primarily caused by two major conditions associated with diabetes: neuropathy and peripheral arterial disease. Neuropathy leads to a loss of sensation in the feet, making it difficult for patients to feel pain or detect injuries. On the other hand, peripheral arterial disease affects blood circulation, slowing down the healing process of any wounds.
The synergy between high blood sugar levels and these complications creates a fertile ground for the rapid progression of foot diseases. These high glucose levels can stiffen arteries and form fatty deposits within blood vessels, further complicating blood flow. This cascade of events underscores the importance of regular monitoring and control of blood sugar levels in preventing diabetic foot complications.
Symptoms to Watch For
Early detection of diabetic foot issues hinges on awareness of the key symptoms, which are often overlooked until they become severe. Symptoms can range from skin discoloration, swelling, and temperature changes in the feet to more severe signs like non-healing wounds, infections, and gangrene.
The American Diabetes Association emphasizes the necessity of a thorough foot examination at least annually, which can play a pivotal role in identifying these early symptoms before they escalate into more serious conditions.Patients should be assessed for their risk levels during these examinations.
Factors such as neuropathy, foot deformities, and previous foot ulcers are considered to categorize patients into low, moderate, or high-risk groups. This stratification helps in tailoring the preventative and management strategies appropriately.
Implementing Prevention Strategies
For those categorized at higher risk, implementing rigorous preventative measures is crucial. These include educating patients on the importance of foot hygiene, regular inspection of feet, the use of therapeutic footwear, and immediate attention to any foot injuries. Moreover, high-risk patients might require referrals to foot care specialists who can provide more comprehensive management, as suggested in the guidelines from the ADA report.
Understanding these aspects of diabetic foot care highlights the complex interplay between physiological factors and preventative care. It also underscores the significance of regular professional evaluations, which can substantially mitigate the risk of severe diabetic foot complications. Through this informed approach, patients can maintain better foot health, significantly reducing the risk of debilitating outcomes that often accompany diabetic foot conditions.
Preventative Measures
While the standard recommendations for managing diabetic foot involve regular monitoring and maintaining good foot hygiene, there are deeper, often overlooked aspects that can significantly enhance preventative efforts. These insights delve into the integration of lifestyle modifications, the psychological impact of diabetic foot, and the strategic use of technology in daily management.
Daily Foot Care Tips
Most diabetic foot care guidelines emphasize the basics—washing feet daily, checking for blisters or sores, and wearing proper footwear. However, an often underappreciated aspect is the material of the socks. Diabetics should consider socks made from materials that reduce moisture and friction, thus lowering the risk of fungal infections and blisters which can escalate quickly in diabetic patients. Additionally, the use of padded socks can provide extra cushioning, which helps in distributing pressure more evenly around the foot, thereby preventing ulcers.
Lifestyle Modifications
The typical advice for lifestyle changes usually centers on diet and exercise. But what’s less discussed is the role of stress management in the prevention of diabetic foot complications. Chronic stress can lead to high blood sugar levels by increasing the release of stress hormones like cortisol and adrenaline. These hormones can antagonize insulin and worsen blood glucose control, thus indirectly contributing to conditions conducive to diabetic foot issues. Incorporating stress-reducing practices such as mindfulness, yoga, or even regular therapy can significantly impact overall diabetes management, including foot health.
Furthermore, sleep quality is another critical yet underrated factor. Poor sleep can affect glycemic control and immune function, which in turn impacts wound healing. Encouraging good sleep hygiene and considering medical evaluation for conditions like sleep apnea could be pivotal in preventing diabetic foot complications.
Harnessing Technology
In the age of digital health advancements, the potential of technology in managing diabetic foot is immense yet underutilized. Wearable devices that monitor foot temperature can detect early signs of ulceration due to inflammation and increased skin temperature. Similarly, mobile apps designed to remind patients to perform their daily foot inspections and provide tips for foot care can increase adherence to preventative practices.
Moreover, telemedicine has emerged as a powerful tool, especially significant in the current global health landscape. Virtual consultations can ensure that patients receive timely advice without the need for travel, which can be particularly beneficial for those with mobility issues due to severe diabetic foot complications. This method of care not only adheres to preventative measures but also enhances patient engagement and adherence to treatment protocols.
Educational Outreach and Support
An often-overlooked aspect of prevention is the power of community and educational support. Organizing diabetic support groups where patients can share experiences, challenges, and tips can greatly enhance motivation and compliance with foot care regimens.
Moreover, these groups can serve as a platform for healthcare professionals to disseminate important information and for patients to receive feedback on their care techniques. These additional layers of diabetic foot prevention—emphasizing psychological health, utilizing modern technology, and fostering community support—provide a comprehensive approach that addresses both the physiological and psychological aspects of diabetes care.
By broadening the scope of preventive measures beyond traditional advice, we can offer a more holistic and effective strategy in managing diabetic foot, ultimately leading to better health outcomes and quality of life for those affected.
Treatment Options for Diabetic Foot
Medications and Topical Treatments
Conventional treatment protocols for diabetic foot typically focus on the use of antibiotics and topical agents to manage infections. However, there’s a provocative shift towards considering the early use of advanced biologics, such as growth factor therapies, which promote healing at the cellular level. This approach challenges the traditional reactive methods that wait for problems to manifest severely before intensifying treatment. By adopting a more proactive strategy, it is possible to enhance recovery rates and reduce the severity of infections, thereby redefining the norms of diabetic foot care.
Advanced Wound Care Techniques
The conventional use of Hyperbaric Oxygen Therapy (HBOT) and bioengineered skin grafts is often reserved as a last resort for severe cases. Yet, if these advanced techniques were employed as frontline defenses, they could potentially revolutionize the management of diabetic foot. Early application of these methods could prevent many complications from reaching critical stages, advocating for a paradigm shift from managing severe complications to preventing them. This approach not only challenges traditional treatment timelines but also emphasizes a proactive health management philosophy.
The Role of Professional Healthcare at Home
Traditionally, home healthcare has been viewed primarily as a convenience. However, in the management of diabetic foot, professional healthcare at home should be recognized as an integral component of effective treatment. Regular visits by healthcare professionals can facilitate continuous assessment and timely modifications to treatment plans, preventing severe complications before they necessitate hospitalization. This perspective challenges the conventional hospital-centric approach and underscores the importance of personalized, proactive health management. Emphasizing home healthcare as a necessary service can transform how diabetic foot care is perceived and delivered, promoting better outcomes through consistent, personalized interventions.
Case Studies and Success Stories
Presenting case studies and success stories where early intervention and innovative treatments have resulted in significant recovery can challenge existing biases and encourage a new perspective on diabetic foot care. These narratives demonstrate the effectiveness of aggressive and innovative approaches, countering skepticism and promoting a more experimental and open approach to managing diabetic foot conditions.
By highlighting these success stories, the article not only informs but also inspires patients and healthcare professionals to advocate for and adopt advanced care strategies. This can lead to a broader acceptance and implementation of cutting-edge treatments, ultimately shifting the standard care practices towards more proactive and preventive measures.
These sections aim to provoke thought and encourage the audience to reconsider and embrace advanced, proactive strategies in diabetic foot management, aligning with a more holistic and forward-thinking approach to diabetes care.
When to see a Specialist?
It’s important to be proactive in managing diabetic foot issues due to the increased risk of foot complications in individuals with diabetes. Here are some key indicators that it’s time to see a specialist:
- Persistent pain or discomfort: If you experience ongoing or severe pain in your feet, it’s essential to consult a specialist. Pain might indicate an underlying issue that needs professional attention.
- Changes in skin color or temperature: Any significant changes in the color (e.g., redness, bluish tint, or darkening) or temperature (especially increased warmth or coolness) of your feet can signal circulatory or nerve issues that require specialist care.
- Swelling: Swelling that doesn’t resolve with elevation or rest could be a sign of infection or inflammation.
- Numbness or tingling: Sensations of numbness or a “pins and needles” feeling in your feet can be symptoms of nerve damage (neuropathy) and should be evaluated by a specialist.
- Sores or wounds that do not heal: Ulcers, open wounds, or sores on the feet that are slow to heal are common in diabetes and can develop into more serious infections without proper treatment.
- Infections: Signs of infection, such as pus, foul-smelling discharge, or increased redness and heat, require immediate attention to prevent more severe complications.
- Structural changes to the feet: Any new deformities, such as bunions, hammer toes, or changes in foot shape, should be assessed by a specialist. These can lead to improper foot alignment and increase the risk of injuries.
- Previous foot problems: If you’ve had foot ulcers or amputations in the past, regular check-ups with a specialist are crucial, even if no current symptoms are present.
Conclusion
As we have navigated through the complex landscape of diabetic foot care, it’s clear that the challenge lies not only in treating the condition but also in implementing robust preventative strategies that address the diverse needs of those at risk. The journey from understanding the diabetic foot to actively managing its complications underscores the necessity for a multidisciplinary approach that encompasses a wide range of medical, technological, and educational resources.
Echoing the insights from the American Diabetes Association, “a structured foot examination and risk assessment is crucial for preventing serious diabetic foot complications like ulcers, infections, and amputations”. This recommendation serves as a cornerstone in diabetic foot care, highlighting the imperative for regular assessments to mitigate the risks associated with this debilitating condition.
In addition to these examinations, the importance of classifying patients into accurately defined risk categories cannot be overstated. By identifying those at low, moderate, or high risk, healthcare providers can tailor interventions more effectively, ensuring that each individual receives the appropriate level of care. This personalized approach not only enhances the efficacy of treatment but also underscores the value of prevention through education and regular monitoring.
Furthermore, the role of home healthcare services like those provided by Best DOC Home Healthcare becomes pivotal in this context. By offering specialized care directly to patients’ homes, these services ensure that the necessary interventions are accessible and timely. For those managing diabetic foot, regular visits from healthcare professionals can make a significant difference in the quality of life and the prevention of severe outcomes.