Frozen shoulder, or adhesive capsulitis, is a condition that leads to stiffness and pain in the shoulder joint, often developing gradually and worsening over time if left untreated. While it may be a common topic in orthopedic circles, the personal impact and long-term challenges it presents to sufferers are less frequently discussed, which are crucial for a comprehensive understanding of this debilitating condition.
Firstly, frozen shoulder is not just a physical ailment; it affects multiple facets of an individual’s life. From diminishing the ability to perform simple daily tasks like dressing or reaching overhead to impacting one’s professional life, especially if their job requires physical activity. This broader impact underscores the importance of timely and effective treatment.
Moreover, frozen shoulder predominantly affects individuals between the ages of 40 and 60 and is more common in women and those with certain medical conditions like diabetes or thyroid disorders. This demographic often faces multiple challenges, including managing their career and personal life, and the onset of a frozen shoulder can significantly disrupt their well-being.
The symptoms of frozen shoulder are typically divided into three stages: the freezing stage, where the pain gradually increases and the range of motion starts to decrease; the frozen stage, where the shoulder becomes stiffer and using it becomes more difficult, and the pain might start to diminish; and finally, the thawing stage, where the range of motion begins to improve. Each stage presents its own set of challenges and duration, which can take anywhere from a few months to a few years to fully cycle through, stressing the need for effective management strategies.
Recognizing the depth of impact and the prolonged course of the condition, addressing frozen shoulder with a comprehensive treatment approach becomes crucial. This is where physiotherapy plays an essential role, not only in managing pain and improving mobility but also in empowering patients through education about self-management techniques tailored to their specific needs and lifestyles. The aim of this discussion is not just to explore if physiotherapy can cure frozen shoulder but to delve into how tailored physiotherapy interventions can significantly enhance quality of life and functional independence for those afflicted.
Understanding Frozen Shoulder
Pathophysiology
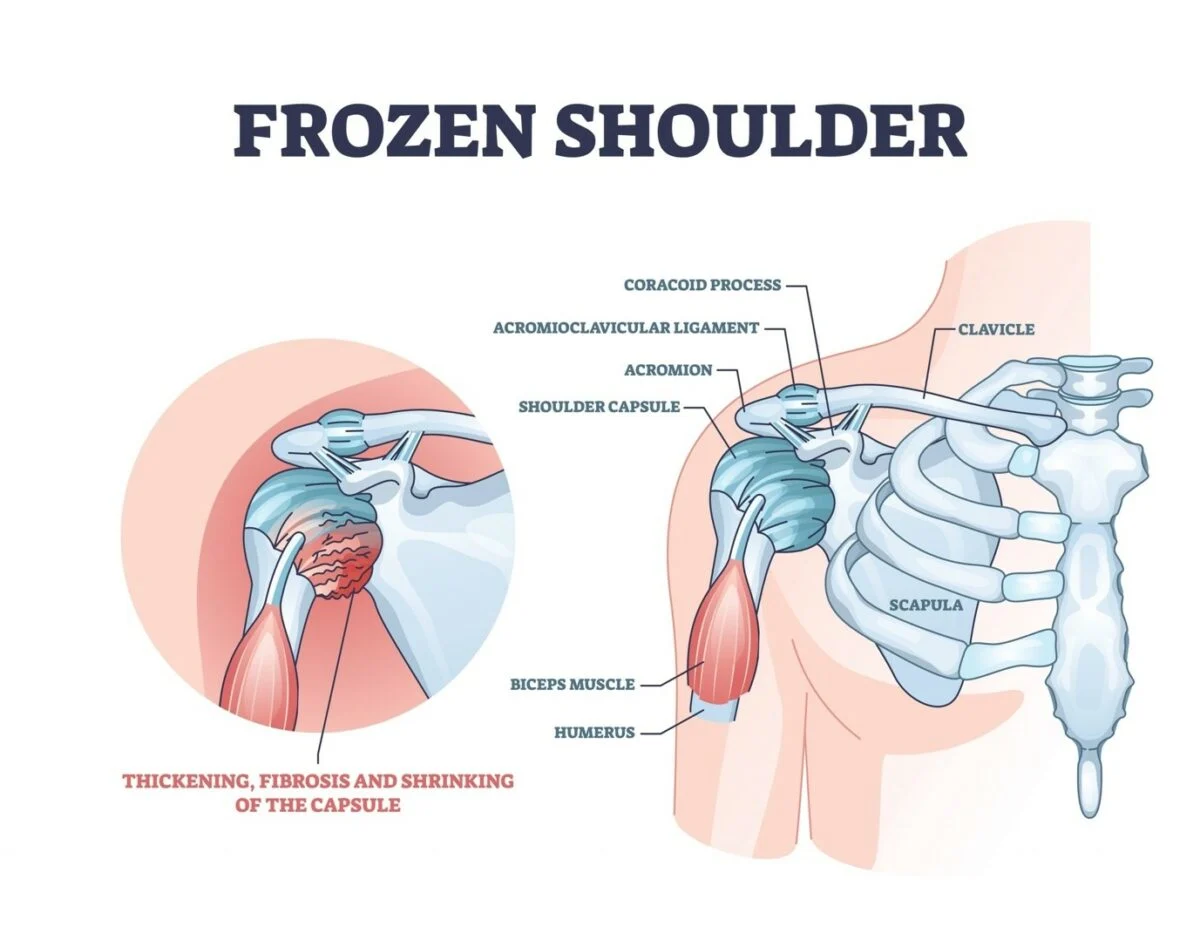
Frozen shoulder, medically termed as adhesive capsulitis, arises from the thickening and tightening of the shoulder capsule, the connective tissue surrounding the glenohumeral joint of the shoulder. This encapsulation restricts movement, leading to chronic pain and a significant reduction in mobility. The exact cause of this fibrotic process remains largely unknown, but it’s hypothesized to involve autoimmune, genetic, and hormonal factors, contributing to an inflammatory response within the joint.
Risk Factors
Certain populations are more susceptible to developing frozen shoulder. Individuals over the age of 40, particularly women, are at a higher risk. Moreover, those with endocrine disorders such as diabetes and thyroid problems, or systemic conditions like cardiovascular disease, are more likely to experience the onset of this condition. A history of shoulder trauma or surgery also increases the risk, as immobility during recovery may lead to joint stiffness.
Stages of Frozen Shoulder
Understanding the stages of frozen shoulder can help in managing expectations and treatment efficacy:
- Freezing Stage: The shoulder becomes painful and range of motion starts to decrease. This stage can last from six weeks to nine months.
- Frozen Stage: Pain may begin to diminish during this stage, but the shoulder becomes stiffer, and using it becomes more difficult. This stage generally lasts four to six months.
- Thawing Stage: Recovery begins, the range of motion gradually returns, and pain decreases. This final stage can last from six months to two years.
A comprehensive review in the National Center for Biotechnology Information outlines the effectiveness of various physiotherapy interventions for treating frozen shoulder. This systematic review analyzed 21 high-quality studies involving 1,249 patients, highlighting significant findings that reinforce the role of physiotherapy:
- Effective Physiotherapy Interventions: The review found that physiotherapy techniques, including manual therapy (like joint mobilization and manipulation), exercise therapy, and electrotherapy, effectively reduce pain and improve both range of motion and overall function.
- Optimal Treatment Combinations: Specifically, the combination of manual therapy techniques and exercise therapy was identified as the most effective physiotherapy approach, optimizing patient outcomes in managing frozen shoulder.
- Recommendation for Physiotherapy: The findings strongly advocate for physiotherapy as a first-line treatment for frozen shoulder, emphasizing its capability to alleviate symptoms and restore shoulder function.
By integrating these insights into treatment plans, physiotherapists can tailor interventions that are not only based on clinical evidence but also adapted to the individual needs and progression stages of the patient’s condition.
The Role of Physiotherapy in Managing Frozen Shoulder
Initial Assessment
The journey towards recovery from frozen shoulder begins with a thorough assessment by a physiotherapist. This step is more than just an evaluation of shoulder mobility; it involves a detailed discussion about the patient’s daily activities, pain levels, and any previous injuries or health conditions. Understanding the patient’s lifestyle and physical demands is crucial as it helps in designing a personalized treatment plan that aligns with their specific needs and goals.
Innovative Physiotherapy Techniques
While traditional techniques such as stretching and strengthening exercises remain foundational in physiotherapy, integrating less conventional, innovative methods can enhance recovery:
- Neuromuscular Electrical Stimulation (NMES): Rarely discussed in mainstream treatment plans for frozen shoulder, NMES can be used to stimulate muscle activity and prevent atrophy in the affected shoulder. It also aids in pain management and muscle re-education.
- Aquatic Therapy: Utilizing the properties of water to reduce load and resistance, aquatic therapy allows for gentle, controlled movements that might be too painful or difficult in a typical setting. This modality is especially beneficial during the freezing stage, as it helps maintain mobility and reduces pain.
- Virtual Reality (VR) Therapy: Emerging as a frontier in physiotherapy, VR can transform how patients perceive their therapy sessions by integrating fun, interactive elements that distract from pain and discomfort. It is especially effective in maintaining patient motivation and engagement throughout the prolonged treatment period typical of frozen shoulder.
Evidence-Based Benefits
Amidst these innovative techniques, it’s essential to ground treatment approaches in evidence-based practice. Recent studies advocate for a combination of manual therapy and exercise, but exploring and documenting the effectiveness of newer modalities can provide fresh insights and possibly improve therapeutic outcomes.
- Integration of Soft Tissue Techniques: Techniques such as myofascial release and trigger point therapy can address the muscle tightness and tenderness that often accompany frozen shoulder, aspects that are sometimes overlooked in traditional physiotherapy plans.
- Customized Exercise Regimens: Beyond generic exercises, physiotherapists can develop bespoke regimens that adapt to the patient’s progress, incorporating real-time feedback and adjusting techniques based on individual response.
The role of physiotherapy in managing frozen shoulder extends beyond mere symptom management; it is about enhancing patient quality of life through innovative, personalized treatment strategies. By pushing the boundaries of traditional physiotherapy and embracing new technologies and methodologies, therapists can offer more than just recovery—they can transform the therapeutic experience, making it as much about healing as it is about personal empowerment and independence.
Case Studies and Success Stories
Redefining Success in Treatment
Conventional measures of success in treating frozen shoulder often focus solely on metrics such as range of motion and pain reduction. While these are undoubtedly important, they can overlook the broader narrative of what recovery means to individual patients. Success should also encompass the ability to return to daily activities and work, improvement in overall quality of life, and patient satisfaction with their progress.
Emphasizing Patient-Centric Outcomes
- Personalized Goals: Success stories in physiotherapy should highlight personalized treatment outcomes. For example, for a painter, regaining the ability to reach overhead to paint a canvas is just as significant as achieving full range of motion. These stories can illustrate how physiotherapy addresses the unique aspects of each patient’s life and career, not just their clinical symptoms.
- Holistic Improvement: Case studies often focus on the immediate effects of physical therapy but may neglect long-term wellness and prevention of future issues. Highlighting how physiotherapy has helped patients incorporate healthy shoulder habits into their lifestyles can inspire a shift from a purely reactive to a proactive approach in healthcare.
Shifting the Narrative with Innovative Examples
- Cross-Disciplinary Approaches: Introducing examples where physiotherapy was combined with other disciplines, such as nutrition or psychology, can challenge the traditional siloed approach to treatment. For instance, integrating dietary advice to reduce inflammation or cognitive-behavioral strategies to cope with the pain and frustration of a slow recovery process.
- Community Engagement: Success stories could also include community involvement or support groups facilitated by physiotherapy clinics, which provide social support and exchange of experiences among patients. This approach fosters a community-based recovery model, emphasizing that healing is not just a physical journey but a communal and emotional one as well.
By broadening the definition of success and introducing holistic, patient-centered narratives, we can inspire a more comprehensive understanding of recovery and encourage a deeper, more meaningful engagement with physiotherapy. These perspectives not only challenge traditional views but also enrich the discourse on healthcare, making it more inclusive and aligned with the diverse needs of patients.
Additional Supportive Treatments
Complementary Therapies
While physiotherapy stands as the cornerstone for treating frozen shoulder, integrating lesser-known supportive treatments can enhance the therapeutic effect and accelerate recovery. These complementary therapies often fly under the radar in conventional discussions but can provide substantial benefits:
- Aromatherapy: The use of essential oils, such as lavender or peppermint, in conjunction with physiotherapy sessions, can aid in reducing pain and anxiety levels. Aromatherapy is believed to stimulate the smell receptors in the nose, which send messages through the nervous system to the brain’s limbic system, affecting moods and emotions. This can be particularly useful in alleviating the stress associated with prolonged treatment for frozen shoulder.
- Sound Therapy: Utilizing sound waves at certain frequencies can help in reducing muscle tension and pain. Sound therapy is thought to help in resetting the muscle tone of hypertonic (overly tight) muscles, which are common in the freezing stage of adhesive capsulitis.
Lifestyle Modifications
Experts often overlook the role of simple lifestyle modifications that can support the physiotherapy treatment plan:
- Ergonomic Adjustments: For patients who work in office settings or perform repetitive shoulder movements, ergonomic adjustments can prevent aggravations of the condition. Simple changes in the workstation setup or the introduction of frequent micro-breaks can make a significant difference in managing symptoms and preventing further injury.
- Dietary Considerations: Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and phytonutrients can support the body’s natural healing processes. Nutrition is seldom discussed in the context of physiotherapy for musculoskeletal disorders, but it can play a critical role in reducing inflammation and promoting tissue healing.
These additional therapies and lifestyle adjustments offer a holistic approach to treating frozen shoulder, emphasizing the importance of addressing both the physical and environmental factors contributing to the condition. By considering these often-neglected areas, healthcare professionals can provide a more comprehensive treatment plan that not only targets the symptoms but also enhances the overall well-being of the patient.
Overcoming Challenges in Physiotherapy for Frozen Shoulder
Patient Compliance Issues
One of the most significant challenges in treating frozen shoulder through physiotherapy is ensuring patient compliance with prescribed exercises and treatment regimens. The conventional view often places the onus of compliance solely on patients, but rethinking this responsibility can lead to better outcomes.
- Empathy in Practice: Instead of merely instructing patients, therapists should aim to build an empathetic understanding of the difficulties patients face. Recognizing the emotional and physical pain involved allows therapists to adjust treatments to be more patient-friendly and less daunting, thereby improving adherence.
- Incorporating Technology: Utilizing apps and virtual trackers that remind patients to perform exercises and allow them to log their pain levels and progress can significantly enhance compliance. These tools not only serve as reminders but also help patients see their progress over time, which can be highly motivating.
Adjusting Treatments Over Time
Frozen shoulder treatment is not a one-size-fits-all solution. Each patient’s journey through the stages of this condition is unique, and their treatment plan needs to reflect this dynamic nature.
- Responsive Treatment Plans: By adopting a more flexible approach to treatment, physiotherapists can adjust therapy based on real-time patient feedback and progress. This approach requires a shift from rigid protocols to more fluid, patient-responsive strategies.
- Integrative Techniques: Combining conventional physiotherapy with innovative treatments such as mindfulness-based stress reduction or yoga can address both the physical and psychological aspects of frozen shoulder. These integrative techniques encourage a holistic recovery and challenge the traditional compartmentalized treatment methods.
Conclusion
As we navigate the complexities of treating frozen shoulder, it is evident that physiotherapy stands out as a pivotal element in managing this condition effectively. The synthesis of clinical research and patient testimonies underscores its critical role. According to a comprehensive review published in the National Center for Biotechnology Information, “Physiotherapy, including manual therapy techniques, exercise therapy, and electrotherapy, was found to be effective in reducing pain and improving range of motion and function in patients with frozen shoulder.” This endorsement of physiotherapy’s efficacy highlights its necessity as a first-line treatment.
The journey through frozen shoulder is undeniably challenging. The condition not only tests physical endurance but also emotional resilience. Yet, with tailored physiotherapy interventions—characterized by a combination of manual therapy and exercise—patients can achieve significant relief and a return to normalcy. The findings of the systematic review reinforce this perspective, showing that specific physiotherapeutic interventions can substantially improve outcomes for those suffering from this debilitating condition.
As we conclude, it’s important to remember that the treatment of frozen shoulder requires more than just physical healing; it necessitates a holistic approach that addresses the full spectrum of the patient’s needs. The integration of innovative techniques and tools, patient education, and a compassionate approach can transform the treatment experience, making recovery not only a possibility but a reality.
Encouraging those affected to seek out skilled physiotherapists who can offer personalized care plans is essential. At Best DOC Home Healthcare, we are committed to providing such expertise directly to your home, ensuring that every aspect of care is handled with precision and empathy. Our services are not just about alleviating symptoms but about restoring confidence and functionality to your life.
“Physiotherapy should be considered a first-line treatment option for frozen shoulder, as it can significantly improve symptoms and restore shoulder function,” states the NCBI article. This powerful assertion is a call to action for patients and healthcare providers alike to embrace physiotherapy as a cornerstone of treatment for frozen shoulder. With the right support and interventions, recovery is not just a hope; it’s an expectation.